Сравнение измерения линейного размера и объёма лёгочных очагов по данным скрининга рака лёгких с помощью низкодозной компьютерной томографии
- Авторы: Сучилова М.М.1, Блохин И.А.1, Алёшина О.О.2, Гомболевский В.А.3, Решетников Р.В.1, Босин В.Ю.1, Омелянская О.В.1, Владзимирский А.В.1,4
-
Учреждения:
- Научно-практический клинический центр диагностики и телемедицинских технологий
- Государственная клиническая больница № 13
- Институт искусственного интеллекта
- Первый Московский государственный медицинский университет имени И.М. Сеченова (Сеченовский Университет)
- Выпуск: Том 4, № 1 (2023)
- Страницы: 5-13
- Раздел: Оригинальные исследования
- URL: https://bakhtiniada.ru/DD/article/view/146871
- DOI: https://doi.org/10.17816/DD117481
- ID: 146871
Цитировать
Аннотация
Обоснование. Согласно результатам голландско-бельгийского исследования скрининга рака лёгких NELSON, измерение объёма (волюметрия) очагов позволяет снизить распространённость ложноположительных результатов до 2,1%.
Цель ― сравнение диагностической точности и согласованности результатов ручного измерения линейного размера с полуавтоматическим измерением объёма очагов по данным пилотного проекта «Московский скрининг рака лёгкого» с использованием низкодозной компьютерной томографии.
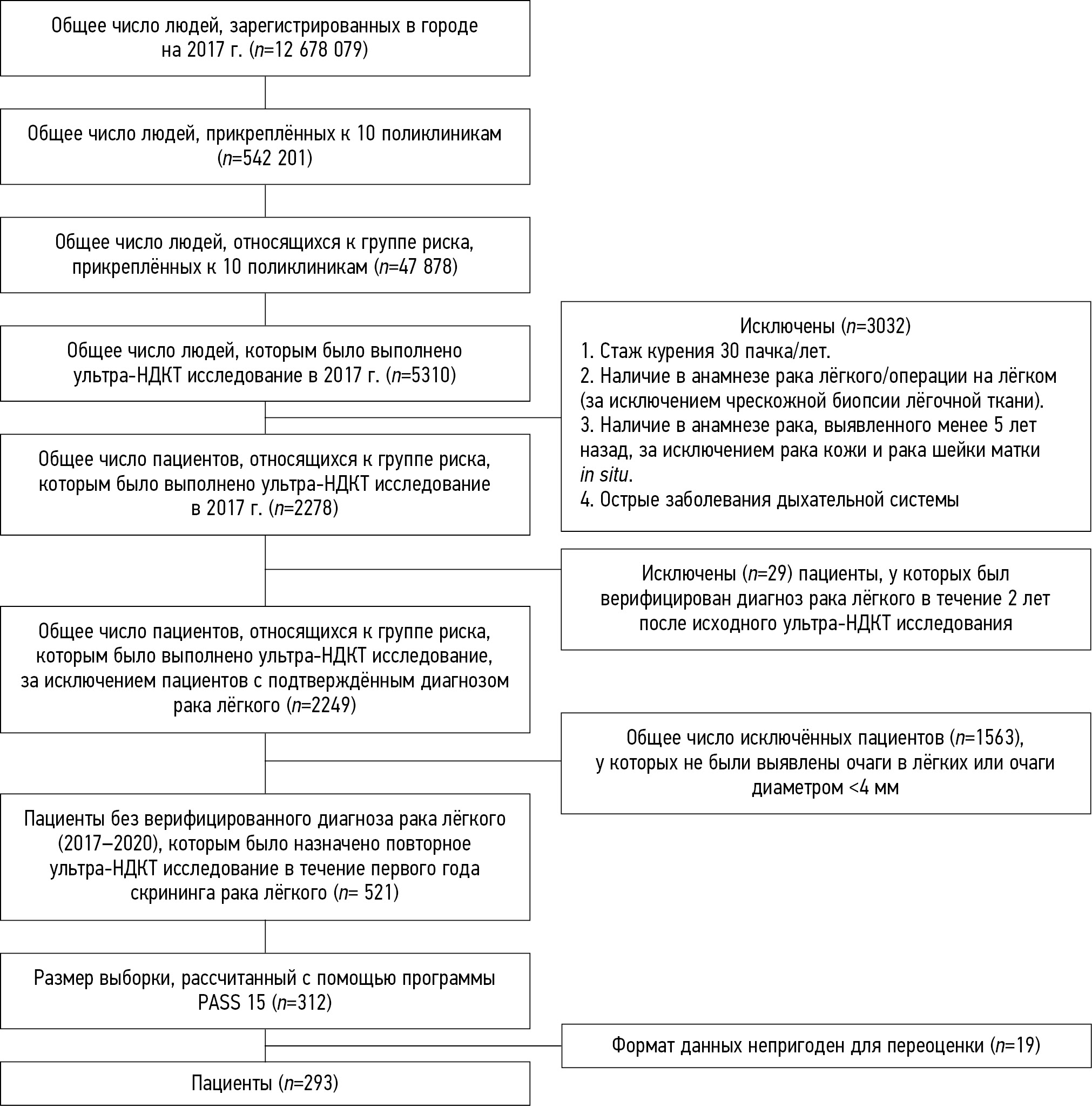
Материалы и методы. В программу скрининга были включены 293 пациента без верифицированного до 2020 года диагноза рака лёгкого, у которых на первичной низкодозной компьютерной томографии, выполненной в период с февраля 2017 по февраль 2018 года, был выявлен очаг в лёгком размером не менее 4 мм. Лучевая нагрузка подбиралась индивидуально и не превышала 1 мЗв. Все изображения низкодозной компьютерной томографии независимо оценивались тремя экспертами для измерения длинной оси очага, а также экстраполированного объёма. В качестве референсного значения размера и объёма брали среднее, полученное по итогам измерений экспертов. Очаг <6 мм/<100 мм3 признавали ложноположительным результатом, очаг ≥6 мм/≥100 мм3 ― ложноотрицательным.
Результаты. В исследование были включены 293 пациента (166 мужчин; 56%; средний возраст 64,6±5,3 года). Лёгочных очагов <6 мм/<100 мм3 было 199. Экспертами 1, 2 и 3 при измерении объёма зафиксированы отличия от референсного стандарта по 32 [10,9%; 4 ложноположительных, 28 ложноотрицательных], 29 [9,9%; 17 ложноположительных, 12 ложноотрицательных] и 30 [10,2%; 6 ложноположительных, 24 ложноотрицательных] очагам, а также расхождения при измерении линейного размера по 92 [65,5%; 107 ложноположительных, 85 ложноотрицательных], 146 [49,8%; 58 ложноположительных, 88 ложноотрицательных] и 102 [34,8%; 23 ложноположительных, 79 ложноотрицательных] очагам соответственно.
Заключение. Использование волюметрии лёгочных очагов значительно снижает количество ложноположительных и ложноотрицательных результатов в сравнении с измерением линейного размера очагов в программе скрининга рака лёгких методом низкодозной компьютерной томографии.
Ключевые слова
Полный текст
Открыть статью на сайте журналаОб авторах
Мария Максимовна Сучилова
Научно-практический клинический центр диагностики и телемедицинских технологий
Автор, ответственный за переписку.
Email: m.suchilova@npcmr.ru
ORCID iD: 0000-0003-1117-0294
SPIN-код: 4922-1894
MD
Россия, МоскваИван Андреевич Блохин
Научно-практический клинический центр диагностики и телемедицинских технологий
Email: i.blokhin@npcmr.ru
ORCID iD: 0000-0002-2681-9378
SPIN-код: 3306-1387
MD
Россия, МоскваОльга Олеговна Алёшина
Государственная клиническая больница № 13
Email: olya.aleshina.tula@gmail.com
ORCID iD: 0000-0001-9924-0204
SPIN-код: 6004-2422
MD
Россия, МоскваВиктор Александрович Гомболевский
Институт искусственного интеллекта
Email: gombolevskiy@npcmr.ru
ORCID iD: 0000-0003-1816-1315
SPIN-код: 6810-3279
к.м.н.
Россия, МоскваРоман Владимирович Решетников
Научно-практический клинический центр диагностики и телемедицинских технологий
Email: reshetnikov@fbb.msu.ru
ORCID iD: 0000-0002-9661-0254
SPIN-код: 8592-0558
к.ф.-м.н.
Россия, МоскваВиктор Юрьевич Босин
Научно-практический клинический центр диагностики и телемедицинских технологий
Email: bosin@npcmr.ru
ORCID iD: 0000-0002-4619-2744
SPIN-код: 3380-7889
д.м.н.
Россия, МоскваОльга Васильевна Омелянская
Научно-практический клинический центр диагностики и телемедицинских технологий
Email: o.omelyanskaya@npcmr.ru
ORCID iD: 0000-0002-0245-4431
SPIN-код: 8948-6152
Россия, Москва
Антон Вячеславович Владзимирский
Научно-практический клинический центр диагностики и телемедицинских технологий; Первый Московский государственный медицинский университет имени И.М. Сеченова (Сеченовский Университет)
Email: a.vladzimirskiy@npcmr.ru
ORCID iD: 0000-0002-2990-7736
SPIN-код: 3602-7120
д.м.н.
Россия, Москва; МоскваСписок литературы
- De Koning H.J., van der Aalst C.M., de Jong P.A., et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial // New Eng J Med. 2020. Vol. 382, N 6. Р. 503–513. doi: 10.1056/NEJMoa1911793
- Henschke C.I., Boffetta P., Yankelevitz D.F., Altorki N. Computed tomography screening: The International Early Lung Cancer Action Program Experience // Thoracic Sur Clin. 2015. Vol. 25, N 2. Р. 129–143. doi: 10.1016/j.thorsurg.2014.12.001
- Callister M.E., Baldwin D.R., Akram A.R., et al. Correction: British Thoracic Society guidelines for the investigation and management of pulmonary nodules: Accredited by NICE // Thorax. 2015. Vol. 70, Suppl 2. Р. ii1–ii54. doi: 10.1136/thoraxjnl-2015-207168
- Oudkerk M., Devaraj A., Vliegenthart R., et al. European Position Statement on Lung Cancer Screening // Lancet Oncology. 2017. Vol. 18, N 12. Р. e754–e766. doi: 10.1016/S1470-2045(17)30861-6
- Wood D.E., Kazerooni E.A., Baum S.L., et al. Lung cancer screening, version 3.2018, NCCN clinical practice guidelines in oncology // J Nation Compr Can Netw. 2018. Vol. 16, N 4. Р. 412–441. doi: 10.6004/jnccn.2018.0020
- Horeweg N., Scholten E.T., de Jong P.A., et al. Detection of lung cancer through low-dose CT screening (NELSON): A prespecified analysis of screening test performance and interval cancers // Lancet Oncology. 2014. Vol. 15, N 12. Р. 1342–1350. doi: 10.1016/S1470-2045(14)70387-0
- Oudkerk M., Liu S., Heuvelmans M.A., et al. Lung cancer LDCT screening and mortality reduction: Evidence, pitfalls and future perspectives // Nat Rev Clin Oncol. 2021. Vol. 18, N 3. Р. 135–151. doi: 10.1038/s41571-020-00432-6
- Duffy S.W., Field J.K. Mortality reduction with low-dose CT screening for lung cancer // New Eng J Med. 2020. Vol. 382, N 6. Р. 572–573. doi: 10.1056/NEJMe1916361
- Морозов С.П., Кузьмина Е.С., Ветшева Н.Н., и др. Московский скрининг: скрининг рака лёгкого с помощью низкодозовой компьютерной томографии // Проблемы социальной гигиены, здравоохранения и истории медицины. 2019. Т. 27, № S. С. 630–636. doi: 10.32687/0869-866X-2019-27-si1-630-636
- Гомболевский В.А., Барчук А.А., Лайпан А.Ш., и др. Организация и эффективность скрининга злокачественных новообразований легких методом низкодозной компьютерной томографии // Радиология-практика. 2018. № 1. С. 28–36.
- Landis J.R., Koch G.G. The measurement of observer agreement for categorical data // Biometrics. 1977. Vol. 33, N 1. Р. 159–174.
- Revel M.P., Bissery A., Bienvenu M., et al. Are two-dimensional CT measurements of small noncalcified pulmonary nodules reliable? // Radiology. 2004. Vol. 231, N 2. Р. 453–458. doi: 10.1148/radiol.2312030167
- Xie X., Willemink M.J., Zhao Y., et al. Inter-and intrascanner variability of pulmonary nodule volumetry on low-dose 64-row CT: An anthropomorphic phantom study // Brit J Radiol. 2013. Vol. 86, N 1029. Р. 20130160. doi: 10.1259/bjr.20130160
- Кульберг Н.С., Решетников Р.В., Новик В.П., и др. Вариабельность заключений при интерпретации КТ-снимков: один за всех и все за одного // Digital Diagnostics. 2021. Т. 2, № 2. С. 105–118. doi: 10.17816/DD60622
Дополнительные файлы