Возможности применения технологий виртуальной и дополненной реальности в современной кардиологии и кардиохирургии
- Авторы: Рашидова С.С.1, Бдоян Э.А.2, Тимурзиева М.М.3, Лобановская С.А.3, Науменко В.В.2, Рахманова А.В.2, Тимофеева В.Д.4, Гуцуляк А.С.5, Зайнуллин А.А.5, Узбекова К.Р.5, Харитонова В.А.5, Ахметова Н.Ф.5
-
Учреждения:
- Перинатальный центр г. Хасавюрта
- Ростовский государственный медицинский университет
- Российский национальный исследовательский медицинский университет имени Н.И. Пирогова
- Первый Санкт-Петербургский государственный медицинский университет имени академика И.П. Павлова
- Башкирский государственный медицинский университет
- Выпуск: Том 5, № 4 (2024)
- Страницы: 819-832
- Раздел: Обзоры
- URL: https://bakhtiniada.ru/DD/article/view/309840
- DOI: https://doi.org/10.17816/DD635577
- ID: 309840
Цитировать
Аннотация
Технологические инновации произвели революцию в медицинской практике, особенно в области кардиохирургии, где сложный характер вмешательств требует точности и предусмотрительности. Использование виртуальной и дополненной реальности в этой области открывает огромные перспективы для улучшения предоперационного планирования, повышения качества медицинского образования и, в конечном счёте, улучшения результатов лечения пациентов.
В данном обзоре проанализирована литература, посвящённая роли виртуальной и дополненной реальности в современной кардиологии, а также обсуждаются возможные направления развития данной области.
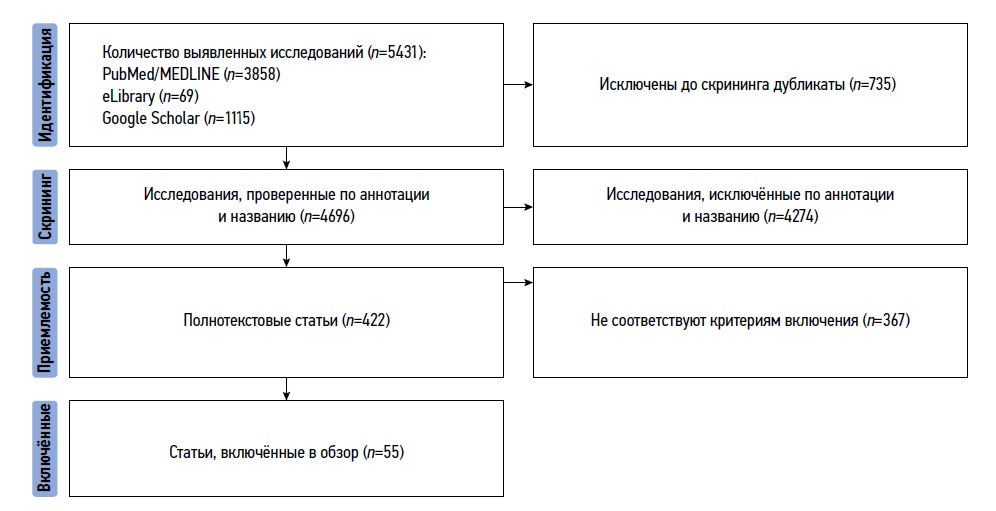
В результате поиска извлечено 3858 публикаций из PubMed/MEDLINE, 69 публикаций из eLibrary и 1115 публикаций, найденных с помощью Google Scholar. Поисковые запросы включали следующие ключевые слова и их сочетания: виртуальная реальность; дополненная реальность; кардиология; кардиохирургия; virtual reality; augmented reality; cardiology; cardiac surgery. Временной интервал поиска: с момента основания соответствующих баз данных по май 2024 года.
Современная кардиологическая помощь включает в себя всё более сложные процедуры, требующие высокого уровня квалификации. Виртуальная реальность становится мощным инструментом как для предпроцедурного планирования, так и для образовательных мероприятий. Она открывает новые возможности для обучения и подготовки специалистов в области кардиологии. С её помощью можно создавать реалистичные симуляции различных ситуаций, с которыми врачи могут столкнуться в своей работе. Это позволяет обучающимся получить практический опыт без риска для реальных пациентов. Интеграция виртуальной реальности в кардиологическую практику имеет большой потенциал, однако для этого необходимо решить ряд проблем. Следует разработать стандарты безопасности и эффективности использования виртуальной реальности в медицинских целях. Также необходимо провести дополнительные исследования, чтобы оценить долгосрочные последствия её использования для здоровья пациентов.
Ключевые слова
Полный текст
Открыть статью на сайте журналаОб авторах
Седа Сулеймановна Рашидова
Перинатальный центр г. Хасавюрта
Автор, ответственный за переписку.
Email: rrstr1990@mail.ru
ORCID iD: 0009-0002-9090-0688
SPIN-код: 5824-7314
врач
Россия, ХасавюртЭмма Альбертовна Бдоян
Ростовский государственный медицинский университет
Email: emma.bdoyan@mail.ru
ORCID iD: 0009-0002-4343-1049
Россия, Ростов-на-Дону
Мадина Мухарбековна Тимурзиева
Российский национальный исследовательский медицинский университет имени Н.И. Пирогова
Email: timurziyeva.madina@bk.ru
ORCID iD: 0009-0002-6048-7108
Россия, Москва
Софья Александровна Лобановская
Российский национальный исследовательский медицинский университет имени Н.И. Пирогова
Email: sonyalobanovsk11@yandex.ru
ORCID iD: 0009-0009-7486-0672
Россия, Москва
Валерия Викторовна Науменко
Ростовский государственный медицинский университет
Email: valerianaumenko555@gmail.com
ORCID iD: 0009-0000-3836-9231
Россия, Ростов-на-Дону
Ангелина Вадимовна Рахманова
Ростовский государственный медицинский университет
Email: alyarakhmanova@mail.ru
ORCID iD: 0009-0002-2209-8988
Россия, Ростов-на-Дону
Валерия Дмитриевна Тимофеева
Первый Санкт-Петербургский государственный медицинский университет имени академика И.П. Павлова
Email: timofeeva-valera@mail.ru
ORCID iD: 0009-0000-0040-6447
Россия, Санкт-Петербург
Алексей Сергеевич Гуцуляк
Башкирский государственный медицинский университет
Email: alex.guculyak@gmail.com
ORCID iD: 0009-0002-3242-9859
врач
Россия, УфаАртем Артурович Зайнуллин
Башкирский государственный медицинский университет
Email: artem.z011@mail.ru
ORCID iD: 0000-0003-1581-7120
Россия, Уфа
Карина Рустамовна Узбекова
Башкирский государственный медицинский университет
Email: uzkarina@mail.ru
ORCID iD: 0009-0009-7099-2635
SPIN-код: 7263-6262
Россия, Уфа
Валерия Артуровна Харитонова
Башкирский государственный медицинский университет
Email: valeriya0901@bk.ru
ORCID iD: 0009-0009-0978-2997
Россия, Уфа
Нарина Фаритовна Ахметова
Башкирский государственный медицинский университет
Email: junehiltoncamp@gmail.com
ORCID iD: 0000-0003-0073-4672
SPIN-код: 7830-7828
Россия, Уфа
Список литературы
- Николаев В.А., Николаев А.А. Опыт и перспективы использования технологий виртуальной, дополненной и смешанной реальности в условиях цифровой трансформации системы здравоохранения // Медицинские технологии. Оценка и выбор. 2020. № 2. С. 35–42. EDN: AWZZTL doi: 10.17116/medtech20204002135
- Jiang Z., Guo Y., Wang Z. Digital twin to improve the virtual real integration of industrial IoT // J Ind Inf Integr. 2021. Vol. 22, N 11. P. 100196. doi: 10.1016/j.jii.2020.100196
- Никитин А.И., Абрамов М.К. Применение VR в медицине. В кн.: Актуальные проблемы авиации и космонавтики. Сборник материалов V Международной научно-практической конференции, посвященной Дню космонавтики. 2019. Т. 2. C. 193–194. EDN: RLBTYQ
- Haleem A., Javaid M. Industry 5.0 and its applications in orthopaedics // J Clin Orthop Trauma. 2019. Vol. 10, N 4. P. 807–808. doi: 10.1016/j.jcot.2018.12.010
- Cho K.H., Hong M.R., Song W.K. Upper Limb Robot Assisted Therapy Based on Visual Error Augmentation in Virtual Reality for Motor Recovery and Kinematics after Chronic Hemiparetic Stroke: A Feasibility Study // Healthcare (Basel). 2022. Vol. 10, N 7. P. 1186. doi: 10.3390/healthcare10071186
- Намиот Е.Д. Дополненная реальность в медицине // International Journal of Open Information Technologies. 2019. Т. 7, № 11. С. 94–99. EDN: ULRJCX
- Sutherland J., Belec J., Sheikh A., et al. Applying Modern Virtual and Augmented Reality Technologies to Medical Images and Models // J Digit Imaging. 2019. Vol. 32, N 1. P. 38–53. doi: 10.1007/s10278-018-0122-7
- Taghian A., Abo Zahhad M., Sayed M.S., Abd El Malek A.H. Virtual and augmented reality in biomedical engineering // Biomed Eng Online. 2023. Vol. 22, N 1. P. 76. doi: 10.1186/s12938-023-01138-3
- Buytaert J.A., Dirckx J.J. Design and quantitative resolution measurements of an optical virtual sectioning three dimensional imaging technique for biomedical specimens, featuring two micrometer slicing resolution // J Biomed Opt. 2007. Vol. 12, N 1. P. 014039. doi: 10.1117/1.2671712
- Silva J.N.A., Southworth M., Raptis C., Silva J. Emerging Applications of Virtual Reality in Cardiovascular Medicine // JACC Basic Transl Sci. 2018. Vol. 3, N 3. P. 420–430. doi: 10.1016/j.jacbts.2017.11.009
- Rymuza B., Grodecki K., Kamiński J., et al. Holographic imaging during transcatheter aortic valve implantation procedure in bicuspid aortic valve stenosis // Kardiol Pol. 2017. Vol. 75, N 10. P. 1056. doi: 10.5603/KP.2017.0195
- Aslani N., Behmanesh A., Garavand A., et al. The Virtual Reality Technology Effects and Features in Cardiology Interventions Training: A Scoping Review // Med J Islam Repub Iran. 2022. Vol. 36. P. 77. doi: 10.47176/mjiri.36.77
- Southworth M.K., Silva J.R., Silva J.N.A. Use of extended realities in cardiology // Trends Cardiovasc Med. 2020. Vol. 30, N 3. P. 143–148. doi: 10.1016/j.tcm.2019.04.005
- Culbertson C., Nicolas S., Zaharovits I., et al. Methamphetamine craving induced in an online virtual reality environment // Pharmacol Biochem Behav. 2010. Vol. 96, N 4. P. 454–460. doi: 10.1016/j.pbb.2010.07.005
- Arslan F., Gerckens U. Virtual support for remote proctoring in TAVR during COVID-19 // Catheter Cardiovasc Interv. 2021. Vol. 98, N 5. P. E733–E736. doi: 10.1002/ccd.29504
- Liu J., Al’Aref S.J., Singh G., et al. An augmented reality system for image guidance of transcatheter procedures for structural heart disease // PLoS One. 2019. Vol. 14, N 7. P. e0219174. doi: 10.1371/journal.pone.0219174
- de Jesus Catalã C.A., Pan R., Rossetto Kron Rodrigues M., de Oliveira Freitas N. Virtual Reality Therapy to Control Burn Pain: Systematic Review of Randomized Controlled Trials // J Burn Care Res. 2022. Vol. 43, N 4. P. 880–888. doi: 10.1093/jbcr/irab213
- Salisbury J.P. Using Medical Device Standards for Design and Risk Management of Immersive Virtual Reality for At Home Therapy and Remote Patient Monitoring // JMIR Biomed Eng. 2021. Vol. 6, N 2. P. e26942. doi: 10.2196/26942
- Keshvari M., Yeganeh M.R., Paryad E., et al. The effect of virtual reality distraction on reducing patients’ anxiety before coronary angiography: a randomized clinical trial study // Egypt Heart J. 2021. Vol. 73, N 1. P. 98. doi: 10.1186/s43044-021-00224-y
- Aardoom J.J., Hilt A.D., Woudenberg T., et al. A Preoperative Virtual Reality App for Patients Scheduled for Cardiac Catheterization: Pre Post Questionnaire Study Examining Feasibility, Usability, and Acceptability // JMIR Cardio. 2022. Vol. 6, N 1. P. e29473. doi: 10.2196/29473
- Morgan H., Nana M., Phillips D., Gallagher S. The Effect of a Virtual Reality Immersive Experience Upon Anxiety Levels, Procedural Understanding, and Satisfaction in Patients Undergoing Cardiac Catheterization: The Virtual Cath Trial // J Invasive Cardiol. 2021. Vol. 33, N 9. P. E681–E686. doi: 10.25270/jic/20.00664
- Gökçe E., Arslan S. Effects of virtual reality and acupressure interventions on pain, anxiety, vital signs and comfort in catheter extraction processes for patients undergoing coronary angiography: A randomized controlled trial // Int J Nurs Pract. 2023. Vol. 29, N 6. P. e13176. doi: 10.1111/ijn.13176
- Bruno R.R., Lin Y., Wolff G., et al. Virtual reality assisted conscious sedation during transcatheter aortic valve implantation: a randomised pilot study // EuroIntervention. 2020. Vol. 16, N 12. P. e1014–e1020. doi: 10.4244/EIJ-D-20-00269
- Hermans A.N.L., Betz K., Verhaert D.V.M., et al. 360° Virtual reality to improve patient education and reduce anxiety towards atrial fibrillation ablation // Europace. 2023. Vol. 25, N 3. P. 855–862. doi: 10.1093/europace/euac246
- Chang S.L., Kuo M.J., Lin Y.J., et al. Virtual reality informative aids increase residents’ atrial fibrillation ablation procedures related knowledge and patients’ satisfaction // J Chin Med Assoc. 2021. Vol. 84, N 1. P. 25–32. doi: 10.1097/JCMA.0000000000000464
- Chang S.L., Kuo M.J., Lin Y.J., et al. Virtual reality based preprocedural education increases preparedness and satisfaction of patients about the catheter ablation of atrial fibrillation // J Chin Med Assoc. 2021. Vol. 84, N 7. P. 690–697. doi: 10.1097/JCMA.0000000000000555
- Brewer M.B., Lau D.L., Chu E.A., et al. Virtual reality can reduce anxiety during office based great saphenous vein radiofrequency ablation // J Vasc Surg Venous Lymphat Disord. 2021. Vol. 9, N 5. P. 1222–1225. doi: 10.1016/j.jvsv.2020.12.081
- Goo H.W., Park S.J., Yoo S.J. Advanced Medical Use of Three Dimensional Imaging in Congenital Heart Disease: Augmented Reality, Mixed Reality, Virtual Reality, and Three Dimensional Printing // Korean J Radiol. 2020. Vol. 21, N 2. P. 133–145. doi: 10.3348/kjr.2019.0625
- Stepanenko A., Perez L.M., Ferre J.C., et al. 3D Virtual modelling, 3D printing and extended reality for planning of implant procedure of short term and long term mechanical circulatory support devices and heart transplantation // Front Cardiovasc Med. 2023. Vol. 10. P. 1191705. doi: 10.3389/fcvm.2023.1191705
- Davies R.R., Hussain T., Tandon A. Using virtual reality simulated implantation for fit testing pediatric patients for adult ventricular assist devices // JTCVS Tech. 2020. Vol. 6. P. 134–137. doi: 10.1016/j.xjtc.2020.10.017
- Ramaswamy R.K., Marimuthu S.K., Ramarathnam K.K., et al. Virtual reality guided left ventricular assist device implantation in pediatric patient: Valuable presurgical tool // Ann Pediatr Cardiol. 2021. Vol. 14, N 3. P. 388–392. doi: 10.4103/apc.apc_81_21
- Tautz L., Walczak L., Georgii J., et al. Combining position based dynamics and gradient vector flow for 4D mitral valve segmentation in TEE sequences // Int J Comput Assist Radiol Surg. 2020. Vol. 15, N 1. P. 119–128. doi: 10.1007/s11548-019-02071-4
- Bruckheimer E., Rotschild C. Holography for imaging in structural heart disease // EuroIntervention. 2016. Vol. 12 Suppl X. P. 81–84. doi: 10.4244/EIJV12SXA15
- Currie M.E., McLeod A.J., Moore J.T., et al. Augmented Reality System for Ultrasound Guidance of Transcatheter Aortic Valve Implantation // Innovations (Phila). 2016. Vol. 11, N 1. P. 31–39. doi: 10.1097/IMI.0000000000000235
- Butera G., Sturla F., Pluchinotta F.R., et al. Holographic Augmented Reality and 3D Printing for Advanced Planning of Sinus Venosus ASD/Partial Anomalous Pulmonary Venous Return Percutaneous Management // JACC Cardiovasc Interv. 2019. Vol. 12, N 14. P. 1389–1391. doi: 10.1016/j.jcin.2019.03.020
- Zbroński K., Rymuza B., Scisło P., et al. Augmented reality in left atrial appendage occlusion // Kardiol Pol. 2018. Vol. 76, N 1. P. 212. doi: 10.5603/KP.2018.0017
- Iannotta M., d’Aiello F.A., Van De Bruaene A., et al. Modern tools in congenital heart disease imaging and procedure planning: a European survey // J Cardiovasc Med (Hagerstown). 2024. Vol. 25, N. 1. P. 76–87. doi: 10.2459/JCM.0000000000001569
- Deng S., Wheeler G., Toussaint N., et al. A Virtual Reality System for Improved Image Based Planning of Complex Cardiac Procedures // J Imaging. 2021. Vol. 7, N 8. P. 151. doi: 10.3390/jimaging7080151
- Raimondi F., Vida V., Godard C., et al. Fast track virtual reality for cardiac imaging in congenital heart disease // J Card Surg. 2021. Vol. 36, N 7. P. 2598–2602. doi: 10.1111/jocs.15508
- Kim B., Loke Y.H., Mass P., et al. A Novel Virtual Reality Medical Image Display System for Group Discussions of Congenital Heart Disease: Development and Usability Testing // JMIR Cardio. 2020. Vol. 4, N 1. P. e20633. doi: 10.2196/20633
- Patel N., Costa A., Sanders S.P., Ezon D. Stereoscopic virtual reality does not improve knowledge acquisition of congenital heart disease // Int J Cardiovasc Imaging. 2021. Vol. 37, N 7. P. 2283–2290. doi: 10.1007/s10554-021-02191-6
- Lau I., Gupta A., Sun Z. Clinical Value of Virtual Reality versus 3D Printing in Congenital Heart Disease // Biomolecules. 2021. Vol. 11, N 6. P. 884. doi: 10.3390/biom11060884
- Milano E.G., Pajaziti E., Schievano S., et al. P369 Patient specific virtual reality for education in con genital heart disease // Eur Heart J Cardiovasc Imaging. 2020. Vol. 21, Suppl. 1. doi: 10.1093/ehjci/jez319.218
- Ong C.S., Krishnan A., Huang C.Y., et al. Role of virtual reality in congenital heart disease // Congenit Heart Dis. 2018. Vol. 13, N 3. P. 357–361. doi: 10.1111/chd.12587
- Sadeghi A.H., Maat A.P.W.M., Taverne Y.J.H.J., et al. Virtual reality and artificial intelligence for 3-dimensional planning of lung segmentectomies // JTCVS Tech. 2021. Vol. 7. P. 309–321. doi: 10.1016/j.xjtc.2021.03.016
- van de Woestijne P.C., Bakhuis W., Sadeghi A.H., et al. 3D Virtual Reality Imaging of Major Aortopulmonary Collateral Arteries: A Novel Diagnostic Modality // World J Pediatr Congenit Heart Surg. 2021. Vol. 12, N 6. P. 765–772. doi: 10.1177/21501351211045064
- Franson D., Dupuis A., Gulani V., et al. A System for Real Time, Online Mixed Reality Visualization of Cardiac Magnetic Resonance Images // J Imaging. 2021. Vol. 7, N 12. P. 274. doi: 10.3390/jimaging7120274
- Bindschadler M., Buddhe S., Ferguson M.R., et al. HEARTBEAT4D: An Open source Toolbox for Turning 4D Cardiac CT into VR/AR // J Digit Imaging. 2022. Vol. 35, N 6. P. 1759–1767. doi: 10.1007/s10278-022-00659-y
- Aeckersberg G., Gkremoutis A., Schmitz Rixen T., Kaiser E. The relevance of low-fidelity virtual reality simulators compared with other learning methods in basic endovascular skills training // J Vasc Surg. 2019. Vol. 69, N 1. P. 227–235. doi: 10.1016/j.jvs.2018.10.047
- Andersen N.L., Jensen R.O., Posth S., et al. Teaching ultrasound guided peripheral venous catheter placement through immersive virtual reality: An explorative pilot study // Medicine (Baltimore). 2021. Vol. 100, N 27. P. e26394. doi: 10.1097/MD.0000000000026394
- Arshad I., De Mello P., Ender M., et al. Reducing Cybersickness in 360 Degree Virtual Reality // Multisens Res. 2021. P. 1–17. doi: 10.1163/22134808 bja10066
- Jung C., Wolff G., Wernly B., et al. Virtual and Augmented Reality in Cardiovascular Care: State of the Art and Future Perspectives // JACC Cardiovasc Imaging. 2022. Vol. 15, N 3. P. 519–532. doi: 10.1016/j.jcmg.2021.08.017
- Mahtab E.A.F., Egorova A.D. Current and future applications of virtual reality technology for cardiac interventions // Nat Rev Cardiol. 2022. Vol. 19, N 12. P. 779–780. doi: 10.1038/s41569-022-00789-4
- Pezel T., Coisne A., Bonnet G., et al. Simulation based training in cardiology: State of the art review from the French Commission of Simulation Teaching (Commission d’enseignement par simulation-COMSI) of the French Society of Cardiology // Arch Cardiovasc Dis. 2021. Vol. 114, N 1. P. 73–84. doi: 10.1016/j.acvd.2020.10.004
- Spiegel B., Fuller G., Lopez M., et al. Virtual reality for management of pain in hospitalized patients: A randomized comparative effectiveness trial // PLoS One. 2019. Vol. 14, N 8. P. e0219115. doi: 10.1371/journal.pone.0219115
Дополнительные файлы