Liver function assessment based on hepatobiliary contrast agent-enhanced magnetic resonance imaging
- Authors: Ageeva S.F.1, Sinitsyn V.E.1, Mershina E.A.1, Rucheva N.A.2, Petrova E.I.3
-
Affiliations:
- Lomonosov Moscow State University
- V.I. Shumakov National Medical Research Center of Transplantology and Artificial Organs
- Industry Clinical Diagnostic Center of Gazprom PJSC
- Issue: Vol 5, No 2 (2024)
- Pages: 137-148
- Section: Original Study Articles
- URL: https://bakhtiniada.ru/DD/article/view/264828
- DOI: https://doi.org/10.17816/DD624826
- ID: 264828
Cite item
Abstract
BACKGROUND: Liver function assessment is very important in clinical practice. The use of magnetic resonance imaging for the anatomical and functional evaluation of the liver is possible in actual clinical practice.
AIM: To examine the possibility of using hepatobiliary contrast-enhanced magnetic resonance imaging for the evaluation of liver function.
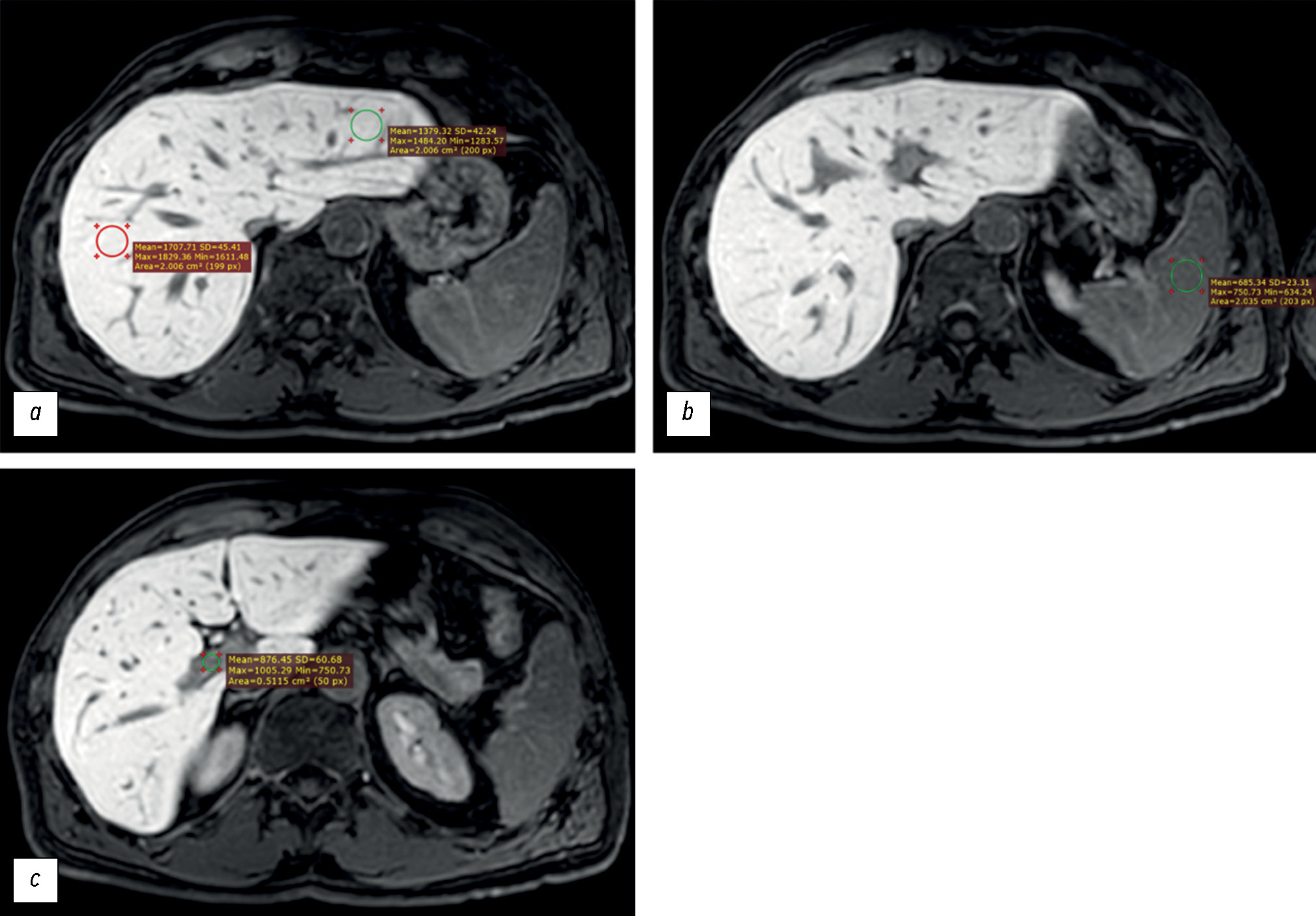
MATERIALS AND METHODS: Datasets of patients who underwent gadoxetic acid-enhanced magnetic resonance imaging were retrospectively reviewed. Patients were divided into two groups: group 1 included patients with impaired liver function, and group 2 included those with normal liver function. Based on magnetic resonance imaging in the hepatobiliary phase, the liver parenchyma signal intensity and its ratio to spleen signal intensity and portal vein signal intensity were estimated. Differences among these parameters were compared between groups. The correlation between liver parenchyma signal intensity and laboratory blood tests reflecting liver function (total bilirubin, albumen, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, gamma glutamyl transpeptidase, and prothrombin time) were analyzed.
RESULTS: Datasets of 53 patients (25 men and 28 women, aged 24–84 years) were analyzed. Group 1 included 19 patients, whereas group 2 included 34. The median liver parenchyma signal intensity was 919.05 [669.65; 1258.35] in group 1 and 1525.13 [1460.5; 1631.4] in group 2 (p=0.0000001). The median ratio of liver parenchyma signal intensity to spleen signal intensity was 1.2 [1.04;1.7] in group 1 and 1.7 [1.46; 1.96] in group 2 (p=0.00076). The median ratio of liver parenchyma signal intensity to portal vein signal intensity was 1.44 [1.29; 1.83] in group 1 and 1.6 [1.43; 1.83] in group 2 (p=0.1). The estimated correlation values between liver parenchyma signal intensity and blood tests parameters were as follows: total bilirubin (r=–0.61; p=0.000001), albumen (r=0.13; p=0.61), aspartate aminotransferase (r=–0.57; p=0.000009), alanine aminotransferase (r=–0.44; p=0.001), alkaline phosphatase (r=–0.45; p=0.0007), gamma glutamyl transpeptidase (r=–0.5; p=0.0003), prothrombin time (r=–0.34; p=0.04).
CONCLUSION: The study reflects the ability to assess liver function using indices (liver parenchyma signal intensity and its ratio to spleen signal intensity) derived from gadoxetic acid-enhanced magnetic resonance imaging. However, this study did not confirm the assumed effectiveness of using the liver parenchyma signal intensity to portal vein signal intensity ratio as an index of liver function. A significant inverse correlation was identified between liver parenchyma signal intensity and blood test parameters in reflecting liver function, except for albumin. The results indicate the possibility of using magnetic resonance imaging to assess liver function.
Keywords
Full Text
##article.viewOnOriginalSite##About the authors
Sofiia F. Ageeva
Lomonosov Moscow State University
Author for correspondence.
Email: son.ageeva13@gmail.com
ORCID iD: 0009-0003-9563-6756
SPIN-code: 9695-3717
Russian Federation, Moscow
Valentin E. Sinitsyn
Lomonosov Moscow State University
Email: vsini@mail.ru
ORCID iD: 0000-0002-5649-2193
SPIN-code: 8449-6590
MD, Dr. Sci. (Medicine), Professor
Russian Federation, MoscowElena A. Mershina
Lomonosov Moscow State University
Email: elena_mershina@mail.ru
ORCID iD: 0000-0002-1266-4926
SPIN-code: 6897-9641
MD, Cand. Sci. (Medicine)
Russian Federation, MoscowNatalia A. Rucheva
V.I. Shumakov National Medical Research Center of Transplantology and Artificial Organs
Email: rna1969@yandex.ru
ORCID iD: 0000-0002-8063-4462
SPIN-code: 2196-8300
MD, Cand. Sci. (Medicine)
Russian Federation, MoscowEkaterina I. Petrova
Industry Clinical Diagnostic Center of Gazprom PJSC
Email: doc_mri@mail.ru
ORCID iD: 0009-0005-0355-8098
MD, Cand. Sci. (Medicine)
Russian Federation, MoscowReferences
- Peng Y, Qi X, Guo X. Child–Pugh Versus MELD Score for the Assessment of Prognosis in Liver Cirrhosis. Medicine. 2016;95(8):e2877. doi: 10.1097/MD.0000000000002877
- Likar YuN, Akhaladze DG, Rumyantsev AG. Hepatobiliary scintigraphy in the preoperative assessment of the future remnant liver function (literature review and own examples). The Russian Journal of Pediatric Hematology аnd Oncology. 2020;7(1):62–69. EDN: VWDZUW doi: 10.21682/2311-1267-2020-7-1-62-69
- Chernyak V, Fowler KJ, Heiken JP, Sirlin CB. Use of gadoxetate disodium in patients with chronic liver disease and its implications for liver imaging reporting and data system (LI-RADS). Journal of Magnetic Resonance Imaging. 2019;49(5):1236–1252. doi: 10.1002/jmri.26540
- Welle CL, Guglielmo FF, Venkatesh SK. MRI of the liver: choosing the right contrast agent. Abdominal Radiology. 2020;45(2):384–392. doi: 10.1007/s00261-019-02162-5
- Furlan A, Borhani AA, Heller MT, Yu RK, Tublin ME. Non-focal liver signal abnormalities on hepatobiliary phase of gadoxetate disodium-enhanced MR imaging: a review and differential diagnosis. Abdominal Radiology. 2016;41(7):1399–1410. doi: 10.1007/s00261-016-0685-z
- Cho SH, Kang UR, Kim JD, Han YS, Choi DL. The value of gadoxetate disodium-enhanced MR imaging for predicting posthepatectomy liver failure after major hepatic resection: A preliminary study. Eur J Radiol. 2011;80(2):e195–e200. doi: 10.1016/j.ejrad.2011.08.008
- Collettini F, Elkilany A, Seta MD, et al. MR imaging of hepatocellular carcinoma: prospective intraindividual head-to-head comparison of the contrast agents gadoxetic acid and gadoteric acid. Sci Rep. 2022;12(1):18583. doi: 10.1038/s41598-022-23397-1
- Galle PR, Forner A, Llovet JM, et al. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi: 10.1016/j.jhep.2018.03.019
- Yang M, Zhang Y, Zhao W, et al. Evaluation of liver function using liver parenchyma, spleen and portal vein signal intensities during the hepatobiliary phase in Gd-EOB-DTPA-enhanced MRI. BMC Med Imaging. 2020;20(1):119. doi: 10.1186/s12880-020-00519-7
- Bastati N, Wibmer A, Tamandl D, et al. Assessment of Orthotopic Liver Transplant Graft Survival on Gadoxetic Acid–Enhanced Magnetic Resonance Imaging Using Qualitative and Quantitative Parameters. Invest Radiol. 2016;51(11):728–734. doi: 10.1097/RLI.0000000000000286
- Mnatsakanyan MK, Rubtsova NA, Kabanov DO, et al. The role of magnetic resonance imaging with gadoxetic acid in the assessment of the functional reserve of the liver. Russian Electronic Journal of Radiology. 2022;12(1):43–55. EDN: GXFGZS doi: 10.21569/2222-7415-2022-12-1-43-55
- Zhang W, Wang X, Miao Y, Hu C, Zhao W. Liver function correlates with liver-to-portal vein contrast ratio during the hepatobiliary phase with Gd-EOB-DTPA-enhanced MR at 3 Tesla. Abdominal Radiology. 2018;43(9):2262–2269. doi: 10.1007/s00261-018-1462-y
- Lee NK, Kim S, Kim GH, et al. Significance of the “Delayed hyperintense portal vein sign” in the hepatobiliary phase MRI obtained with Gd-EOB-DTPA. Journal of Magnetic Resonance Imaging. 2012;36(3):678–685. doi: 10.1002/jmri.23700
- Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707–710. doi: 10.1007/BF01709751
- Zaccherini G, Weiss E, Moreau R. Acute-on-chronic liver failure: Definitions, pathophysiology and principles of treatment. JHEP Reports. 2021;3(1):100176. doi: 10.1016/j.jhepr.2020.100176
Supplementary files