Role of teleradiology in the interpretation of ultrasound images acquired in the emergency setting
- Autores: Kalyanpur A.1, Mathur N.2
-
Afiliações:
- Teleradiology Solutions
- Image Core Lab
- Edição: Volume 5, Nº 2 (2024)
- Páginas: 231-242
- Seção: Original Study Articles
- URL: https://bakhtiniada.ru/DD/article/view/264835
- DOI: https://doi.org/10.17816/DD624586
- ID: 264835
Citar
Resumo
BACKGROUND: Teleradiology has become an important tool in emergency medicine, particularly in the interpretation of emergency ultrasonography. In emergency situations, where time is essential, rapid diagnosis and treatment can mean the difference between life and death. Teleradiology is an innovative alternative to augment the staffing and fill the gaps of onsite radiology personnel in emergency departments or during off-hours.
AIM: To assess the effectiveness/impact of teleradiology in emergency ultrasound interpretation.
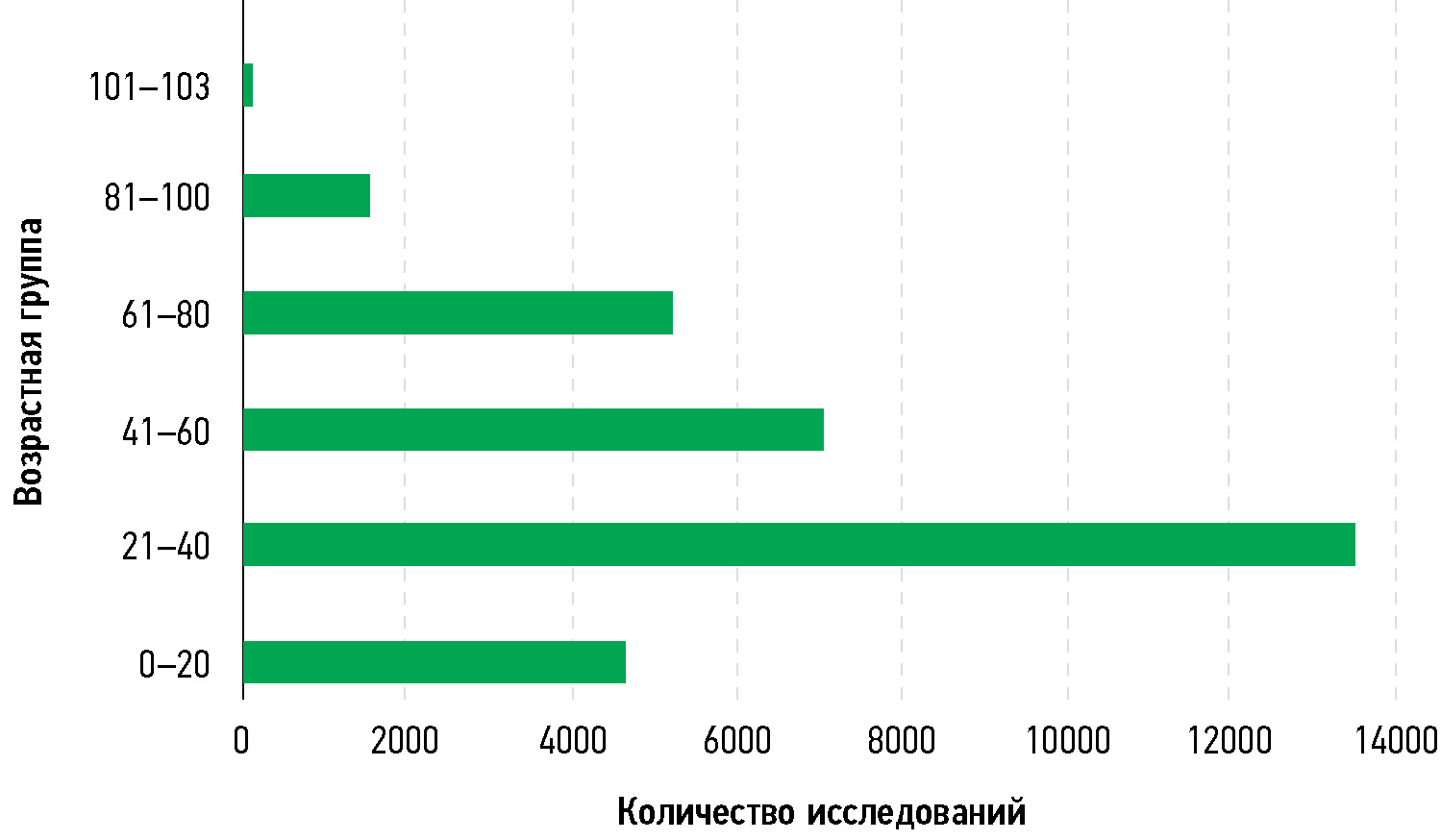
MATERIALS AND METHODS: A retrospective study was performed in a cohort of 33,616 patients from 86 hospitals across the USA between January and December 2022. The study involved radiological interpretations of 37,253 ultrasound images acquired in the emergency setting by American Board Certified Radiologists empaneled by a teleradiology service provider, headquartered in Bangalore, India.
RESULTS: The proposed telehealth model provided timely and quality reporting of 37,253 scans of patients with a mean turnaround time of 35.71 min (95% confidence interval 35.50–35.91).
CONCLUSION: This study demonstrates that a structured telesonography program with defined protocols for image capture, transmission, and clinical communication can allow for successful immediate reporting of ultrasound data in the emergency care setting.
Palavras-chave
Texto integral
##article.viewOnOriginalSite##Sobre autores
Arjun Kalyanpur
Teleradiology Solutions
Email: arjun.kalyanpur@telradsol.com
ORCID ID: 0000-0003-2761-7273
MD
Índia, BangaloreNeetika Mathur
Image Core Lab
Autor responsável pela correspondência
Email: neetika.mathur@imagecorelab.com
ORCID ID: 0009-0002-8884-2060
PhD
Rússia, BangaloreBibliografia
- Kalyanpur A. The role of teleradiology in emergency radiology provision. Radiol Manage. 2014;36(3):46–49.
- Burute N, Jankharia B. Teleradiology: The Indian perspective. Indian Journal of Radiology and Imaging. 2009;19(1):16–18. doi: 10.4103/0971-3026.45337
- Michalke JA. An overview of emergency ultrasound in the United States. World J Emerg Med. 2012;3(2):85–90. doi: 10.5847/wjem.j.issn.1920-8642.2012.02.001
- Misra A, Yadav DC, Kole T. Emergency care in India beyond 75 years of independence — problems and solutions. J Glob Health. 2023;13:03015. doi: 10.7189/jogh.13.03015
- National Hospital Ambulatory Medical Care Survey: 2020 Emergency Department Summary Tables [Internet]. US: National Center for Health Statistics. Available from: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2020-nhamcs-ed-web-tables-508.pdf
- Perotte R, Lewin GO, Tambe U, et al. Improving Emergency Department Flow: Reducing Turnaround Time for Emergent CT Scans. AMIA Annu Symp Proc. 2018;2018:897–906.
- Agrawal A, Khandelwal N. Nucleating emergency radiology specialization in India. Emerg Radiol. 2016;23(2):101–103. doi: 10.1007/s10140-016-1381-6
- Abdolrazaghnejad A, Banaie M, Safdari M. Ultrasonography in Emergency Department; a Diagnostic Tool for Better Examination and Decision-Making. Adv J Emerg Med. 2018;2(1):e7. doi: 10.22114/AJEM.v0i0.40
- Nicola R, Dogra V. Ultrasound: the triage tool in the emergency department: using ultrasound first. Br J Radiol. 2016;89(1061):20150790. doi: 10.1259/bjr.20150790
- Islam SN, Deka N, Hussain Z. Role of Doppler Ultrasound in Assessing the Severity of Peripheral Arterial Diseases of the Lower Limb. J Med Ultrasound. 2021;29(4):277–280. doi: 10.4103/JMU.JMU_137_20
- Kalyanpur A, Meka S, Joshi K, Somashekaran Nair HT, Mathur N. Teleradiology in Tripura: Effectiveness of a Telehealth Model for the Rural Health Sector. International Journal of Health Technology and Innovation. 2022;1:7–12. doi: 10.60142/ijhti.v1i02.36
- Agrawal A. Emergency Teleradiology-Past, Present, and, Is There a Future? Front Radiol. 2022;2:866643. doi: 10.3389/fradi.2022.866643
- Kalyanpur A, Weinberg J, Neklesa V, et al. Emergency radiology coverage: technical and clinical feasibility of an international teleradiology model. Emerg Radiol. 2003;10(3):115–118. doi: 10.1007/s10140-003-0284-5
- Agrawal A, Agrawal A, Pandit M, Kalyanpur A. Systematic survey of discrepancy rates in an international teleradiology service. Emerg Radiol. 2011;18(1):23–29. doi: 10.1007/s10140-010-0899-2
- Chandramohan A, Krothapalli V, Augustin A, et al. Teleradiology and technology innovations in radiology: status in India and its role in increasing access to primary health care. The Lancet Regional Health — Southeast Asia. 2023;23. doi: 10.1016/j.lansea.2023.100195
- Thrall JH. Teleradiology Part I. History and Clinical Applications. Radiology. 2007;243(3):613–617. doi: 10.1148/radiol.2433070350
- Duarte ML, Dos Santos LR, Iared W, Peccin MS. Telementored ultrasonography: a narrative review. Sao Paulo Med J. 2022;140(2):310–319. doi: 10.1590/1516-3180.2020.0607.R2.15092021
- Bergquist HB, Burkholder TW, Muhammad Ali OA, Omer Y, Wallis LA. Considerations for service delivery for emergency care in low resource settings. African Journal of Emergency Medicine. 2020;10:S7–S11. doi: 10.1016/j.afjem.2020.07.002
- Agrawal A, Khandelwal N. Nucleating emergency radiology specialization in India. Emerg Radiol. 2016;23(2):101–103. doi: 10.1007/s10140-016-1381-6
- Fast Facts on U.S. Hospitals [Internet]. US: American Hospital Association. c2024. Available from: https://www.aha.org/statistics/fast-facts-us-hospitals
- Szabo I, Zag L, Takács I, et al. Quantile regression and an application: performance improvement of an emergency department in Eastern Europe. Hungarian Statistical Review. 2020;3(1):60–76. doi: 10.35618/hsr2020.01.en060
- Honig SE, Honig EL, Babiarz LB, et al. Critical findings: timing of notification in neuroradiology. AJNR Am J Neuroradiol. 2014;35(8):1485–1492. doi: 10.3174/ajnr.A3918
Arquivos suplementares