Role of chest MRI for the diagnosis of malignant pulmonary nodules: a systematic review and a meta-analysis
- Authors: Vasilev Y.A.1,2, Panina O.Y.1,2,3, Grik E.A.3, Akhmad K.S.1, Vasileva Y.N.3
-
Affiliations:
- Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of Moscow Health Care
- City Clinical Oncological Hospital No. 1
- Moscow State University of Medicine and Dentistry named after A.I. Evdokimov
- Issue: Vol 2, No 3 (2021)
- Pages: 301-312
- Section: Systematic reviews
- URL: https://bakhtiniada.ru/DD/article/view/70306
- DOI: https://doi.org/10.17816/DD70306
- ID: 70306
Cite item
Abstract
AIM: To evaluate the ability of magnetic resonance imaging (MRI) of the chest to detect malignant pulmonary nodules compared to compute tomography (CT).
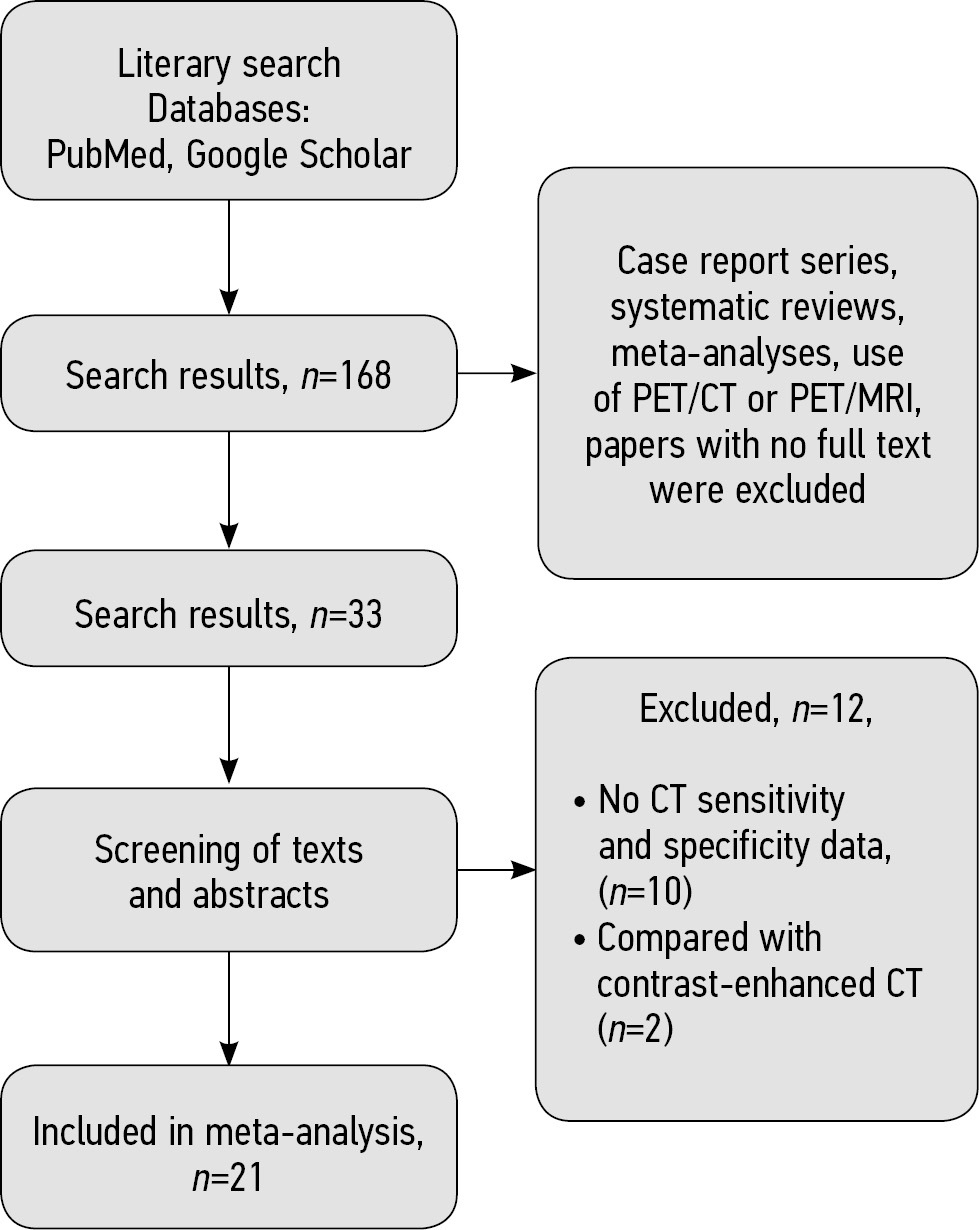
MATERIALS AND METHODS: We searched the following databases with the final date of search on April 7th, 2021: PubMed, Google Scholar. We selected studies according to the inclusion and exclusion criteria that assessed the detection of malignant lung nodules by MRI and CT and included information about sensitivity and specificity. Method of the analysis and data grouping was chosen with regard to statistical heterogeneity of the studies included in the analysis. We used the χ2 test and I2 statistic to evaluate the heterogeneity.
RESULTS: We selected 168 articles for the systematic review from the PubMed and Google Scholar databases. We included 21 studies on 1,188 patients in the meta-analysis and revealed statistically significant heterogeneity (р<0,00001 for χ2 test; I2=99%) for sensitivity and specificity. Hence, we used a random-effect model for further analysis. As a result, values of sensitivity for detection of pulmonary nodules with MRI of 70.4%–100%, specificity ― from 60.6% to 100%.
CONCLUSIONS: Thus, MRI has sufficient sensitivity and specificity for detecting malignant pulmonary nodules primarily discovered with CT.
Keywords
Full Text
##article.viewOnOriginalSite##About the authors
Yuriy A. Vasilev
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of Moscow Health Care; City Clinical Oncological Hospital No. 1
Email: dr.vasilev@me.com
ORCID iD: 0000-0002-0208-5218
SPIN-code: 4458-5608
MD, Cand. Sci. (Med)
Russian Federation, 24/1 Petrovka str., 127051, Moscow; MoscowOlga Y. Panina
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of Moscow Health Care; City Clinical Oncological Hospital No. 1; Moscow State University of Medicine and Dentistry named after A.I. Evdokimov
Email: o.panina@npcmr.ru
ORCID iD: 0000-0002-8684-775X
SPIN-code: 5504-8136
Scopus Author ID: 57219837311
Junior Scientist Researcher
Russian Federation, 24/1 Petrovka str., 127051, Moscow; Moscow; 20, p. 1, Delegatskaya str., Moscow, 127473Evgeniia A. Grik
Moscow State University of Medicine and Dentistry named after A.I. Evdokimov
Email: evgeniyagrik@gmail.com
ORCID iD: 0000-0002-7908-3982
SPIN-code: 5558-7307
MD
Russian Federation, 20/1, Delegatskaya str., Moscow, 127473Kate S. Akhmad
Research and Practical Clinical Center for Diagnostics and Telemedicine Technologies of Moscow Health Care
Email: e.ahmad@npcmr.ru
ORCID iD: 0000-0002-8235-9361
SPIN-code: 5891-4384
Russian Federation, 24/1, Petrovka street,127051 Moscow
Yulia N. Vasileva
Moscow State University of Medicine and Dentistry named after A.I. Evdokimov
Author for correspondence.
Email: drugya@yandex.ru
ORCID iD: 0000-0003-4955-2749
SPIN-code: 9777-2067
MD, Cand. Sci. (Med.)
Russian Federation, 20/1, Delegatskaya str., Moscow, 127473References
- Ost D, Fein AM, Feinsilver SH. Clinical practice. The solitary pulmonary nodule. N Engl J Med. 2003;348(25):2535–2542. doi: 10.1056/NEJMcp012290
- Nasim F, Ost DE. Management of the solitary pulmonary nodule. Curr Opin Pulm Med. 2019;25(4):344–353. doi: 10.1097/MCP.0000000000000586
- MacMahon H, Naidich DP, Goo JM, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: From the Fleischner Society 2017. Radiology. 2017;284(1):228–243. doi: 10.1148/radiol.2017161659
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100
- Whiting PF, Rutjes AW, Westwood ME, et al. Quadas-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536. doi: 10.7326/0003-4819-155-8-201110180-00009
- Higgins JP, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, Hoboken; 2019. doi: 10.1002/9781119536604
- Both M, Schultze J, Reuter M, et al. Fast T1- and T2-weighted pulmonary MR-imaging in patients with bronchial carcinoma. Eur J Radiol. 2005;53(3):478–488. doi: 10.1016/j.ejrad.2004.05.007
- Bruegel M, Gaa J, Woertler K, et al. MRI of the lung: Value of different turbo spin-echo, single-shot turbo spin-echo, and 3D gradient-echo pulse sequences for the detection of pulmonary metastases. J Magn Reson Imaging. 2007;25(1):73–81. doi: 10.1002/jmri.20824
- Meier-Schroers M, Kukuk G, Homsi R, et al. MRI of the lung using the PROPELLER technique: Artifact reduction, better image quality and improved nodule detection. Eur J Radiol. 2016;85(4): 707–713. doi: 10.1016/j.ejrad.2015.12.016
- Meier-Schroers M, Homsi R, Schild HH, Thomas D. Lung cancer screening with MRI: characterization of nodules with different non-enhanced MRI sequences. Acta Radiol. 2019;60(2):168–176. doi: 10.1177/0284185118778870
- Ohno Y, Koyama H, Yoshikawa T, et al. Standard-, reduced-, and nodose thin-section radiologic examinations: Comparison of capability for nodule detection and nodule type assessment in patients suspected of having pulmonary nodules. Radiology. 2017;284(2):562–573. doi: 10.1148/radiol.2017161037
- Regier M, Schwarz D, Henes FO, et al. Diffusion-weighted MR-imaging for the detection of pulmonary nodules at 1.5 Tesla: Intraindividual comparison with multidetector computed tomography. J Med Imaging Radiat Oncol. 2011;55(3):266–274. doi: 10.1111/j.1754-9485.2011.02263.x
- Satoh S, Kitazume Y, Ohdama S, et al. Can malignant and benign pulmonary nodules be differentiated with diffusion-weighted MRI? Am J Roentgenol. 2008;191(2):464–470. doi: 10.2214/AJR.07.3133
- Schaefer JF, Schneider V, Vollmar J, et al. Solitary pulmonary nodules: Association between signal characteristics in dynamic contrast enhanced MRI and tumor angiogenesis. Lung Cancer. 2006;53(1):39–49. doi: 10.1016/j.lungcan.2006.03.010
- Schroeder T, Ruehm SG, Debatin JF, et al. Detection of pulmonary nodules using a 2D HASTE MR sequence: comparison with MDCT. Am J Roentgenol. 2005;185(4):979–984. doi: 10.2214/AJR.04.0814
- Sommer G, Tremper J, Koenigkam-Santos M, et al. Lung nodule detection in a high-risk population: Comparison of magnetic resonance imaging and low-dose computed tomography. Eur J Radiol. 2014;83(3):600–605. doi: 10.1016/j.ejrad.2013.11.012
- Vogt FM, Herborn CU, Hunold P, et al. HASTE MRI versus chest radiography in the detection of pulmonary nodules: comparison with MDCT. Am J Roentgenol. 2004;183(1):71–78. doi: 10.2214/ajr.183.1.1830071
- Yi CA, Jeon TY, Lee KS, et al. 3-T MRI: usefulness for evaluating primary lung cancer and small nodules in lobes not containing primary tumors. Am J Roentgenol. 2007;189(2):386–392. doi: 10.2214/AJR.07.2082
- Chang S, Hong SR, Kim YJ, et al. Usefulness of thin-section single-shot turbo spin echo with half-fourier acquisition in evaluation of local invasion of lung cancer. J Magn Reson Imaging. 2015;41(3):747–754. doi: 10.1002/jmri.24587
- Schaefer JF, Vollmar J, Schick F, et al. Solitary pulmonary nodules: Dynamic contrast-enhanced MR imaging ― Perfusion differences in malignant and benign lesions. Radiology. 2004;232(2):544–553. doi: 10.1148/radiol.2322030515
- Kono R, Fujimoto K, Terasaki H, et al. Dynamic MRI of solitary pulmonary nodules: comparison of enhancement patterns of malignant and benign small peripheral lung lesions. Am J Roentgenol. 2007;188(1):26–36. doi: 10.2214/AJR.05.1446
- Feng H, Shi G, Liu H, et al. Free-breathing radial volumetric interpolated breath-hold examination sequence and dynamic contrast-enhanced MRI combined with diffusion-weighted imaging for assessment of solitary pulmonary nodules. Magn Reson Imaging. 2021;75:100–106. doi: 10.1016/j.mri.2020.10.009
- Kim JH, Kim HJ, Lee KH, et al. Solitary pulmonary nodules: A comparative study evaluated with contrast-enhanced dynamic MR imaging and CT. J Comput Assist Tomogr. 2004;28(6):766–775. doi: 10.1097/00004728-200411000-00007
- Ohno Y, Nishio M, Koyama H, et al. Solitary pulmonary nodules: Comparison of dynamic first-pass contrast-enhanced perfusion area-detector CT, dynamic first-pass contrast-enhanced MR imaging, and FDG PET/CT. Radiology. 2015;274(2):563–575. doi: 10.1148/radiol.14132289
- Heye T, Sommer G, Miedinger D, et al. Ultrafast 3D balanced steady-state free precession MRI of the lung: Assessment of anatomic details in comparison to low-dose CT. J Magn Reson Imaging. 2015;42(3):602–609. doi: 10.1002/jmri.24836
- Akata S, Kajiwara N, Park J, et al. Evaluation of chest wall invasion by lung cancer using respiratory dynamic MRI. J Med Imaging Radiat Oncol. 2008;52(1):36–39. doi: 10.1111/j.1440-1673.2007.01908.x
- Hittmair K, Eckersberger F, Klepetko W, et al. Evaluation of solitary pulmonary nodules with dynamic contrast-enhanced MR imaging-a promising technique? Magn Reson Imaging. 1995;13(7):923–933. doi: 10.1016/0730-725x(95)02010-q
- Alper F, Kurt AT, Aydin Y, et al. The role of dynamic magnetic resonance imaging in the evaluation of pulmonary nodules and masses. Med Princ Pract. 2013;22(1):80–86. doi: 10.1159/000339475
- Frericks BB, Meyer BC, Martus P, et al. MRI of the thorax during whole-body MRI: Evaluation of different MR sequences and comparison to thoracic multidetector computed tomography (MDCT). J Magn Reson Imaging. 2008;27(3):538–545. doi: 10.1002/jmri.21218
- Cieszanowski A, Lisowska A, Dabrowska M, et al. MR imaging of pulmonary nodules: Detection rate and accuracy of size estimation in comparison to computed tomography. PLoS One. 2016;11(6):e0156272. doi: 10.1371/journal.pone.0156272
- Ohno Y, Hatabu H, Takenaka D, et al. Solitary pulmonary nodules: Potential role of dynamic MR imaging in management ― Initial experience. Radiology. 2002;224(2):503–511. doi: 10.1148/radiol.2242010992
- Zou Y, Zhang M, Wang Q, et al. Quantitative investigation of solitary pulmonary nodules: dynamic contrast-enhanced MRI and histopathologic analysis. Am J Roentgenol. 2008;191(1):252–259. doi: 10.2214/AJR.07.2284
- Dewes P, Frellesen C, Al-Butmeh F, et al. Comparative evaluation of non-contrast CAIPIRINHA-VIBE 3T-MRI and multidetector CT for detection of pulmonary nodules: In vivo evaluation of diagnostic accuracy and image quality. Eur J Radiol. 2016;85(1):193–198. doi: 10.1016/j.ejrad.2015.11.020
- Fatihoglu E, Biri S, Aydın S, et al. MRI in evaluation of solitary pulmonary nodules. Turkish Thorac J. 2019;20(2):90–96. doi: 10.5152/TurkThoracJ.2018.18049
- Heye T, Ley S, Heussel CP, et al. Detection and size of pulmonary lesions: How accurate is MRI? A prospective comparison of CT and MRI. Acta Radiol. 2012;53(2):153–160. doi: 10.1258/ar.2011.110445
- Koo CW, Lu A, Takahashi EA, et al. Can MRI contribute to pulmonary nodule analysis? J Magn Reson Imaging. 2019;49(7): e256–e264. doi: 10.1002/jmri.26587
- Koyama H, Ohno Y, Kono A, et al. Quantitative and qualitative assessment of non-contrast-enhanced pulmonary MR imaging for management of pulmonary nodules in 161 subjects. Eur Radiol. 2008;18(10):2120–2131. doi: 10.1007/s00330-008-1001-2
- Koyama H, Ohno Y, Seki S, et al. Value of diffusion-weighted MR imaging using various parameters for assessment and characterization of solitary pulmonary nodules. Eur J Radiol. 2015;84(3):509–515. doi: 10.1016/j.ejrad.2014.11.024
- Huang YS, Niisato E, Su MY, et al. Detecting small pulmonary nodules with spiral ultrashort echo time sequences in 1.5 T MRI. MAGMA. 2021;34(3):399–409. doi: 10.1007/s10334-020-00885-x
- Ying GS, Maguire MG, Glynn RJ,et al. Calculating sensitivity, specificity, and predictive values for correlated eye data. Investig Ophthalmol Vis Sci. 2020;61(11):29. doi: 10.1167/iovs.61.11.29
- Bradley SH, Kennedy MP, Neal RD. Recognising lung cancer in primary care. Adv Ther. 2019;36(1):19–30. doi: 10.1007/s12325-018-0843-5
- Nikolаev E, Gombolevskiy V, Gonchar AP, et al. Incidental findings during lung cancer screening by low-dose computed tomography. Tuberc Lung Dis. 2018;96(11):60–67. doi: 10.21292/2075-1230-2018-96-11-60-67
- Loverdos K, Fotiadis A, Kontogianni C, et al. Lung nodules: A comprehensive review on current approach and management. Ann Thorac Med. 2019;14(4):226–238. doi: 10.4103/atm.ATM_110_19
Supplementary files